People with epilepsy often experience changes in their quality of life such as less mobility, as well as the impact on learning, school attendance, employment, relationships, and social interactions. In order to live a happy and full life it’s important to learn how epilepsy can affect you, what your rights and responsibilities are and how to find support and resources.
The challenges of living with epilepsy may be different for children, adolescents, and seniors than for adults. Visit the sections for Children and Teens, Women, Men and Seniors to explore specific information. If you are an adult with epilepsy and have questions about things like transportation, disability benefits or legal issues, visit our Information for Adults page. As always, the EFEPA staff is here to speak with you about the diverse issues facing people with epilepsy. We can assist you in identifying options for problem solving or refer you to a resource best suited for your needs.
Below you’ll find information on a range of topics:
- What is Epilepsy
- First Aid
- Home Safety
- Treatment Options
- Sleep and Epilepsy
- Mood and Memory *Video*
- Self Esteem *Video*
- Headaches and Epilepsy *Slides*
- For Caregivers: Helping Someone with Epilepsy *Slides*
For a great introduction to living with epilepsy, view this short video with Dr. Sarah Schmitt as she covers topics like Sleep and Epilepsy, Balancing Work and School, Nutrition, Exercise, Special Diets, Bone Health and more.
What is Epilepsy
Epilepsy is the underlying tendency of the brain to produce sudden abnormal bursts of electrical energy that disrupt other brain functions and cause seizures. A seizure happens when a brief, strong surge of electrical activity affects part or all of the brain. When a person has two or more unprovoked seizures, they are considered to have epilepsy. Almost 3.4 million people in the U.S. have some form of epilepsy. About 150,000 new cases of epilepsy are diagnosed each year. In the Eastern Pennsylvania region alone there are over 110,000 people living with epilepsy. Over a lifetime, one in 10 people will have a seizure, and one in 26 will be diagnosed with epilepsy.
Seizures can last from a few seconds to a few minutes. They can have many symptoms, from convulsions and loss of consciousness to more subtle symptoms like blank staring, lip smacking, or jerking movements of arms and legs. Some symptoms of seizures are not always recognized as seizures by the person experiencing them or by health care professionals. Learn more about the different types of seizures here.
First Aid
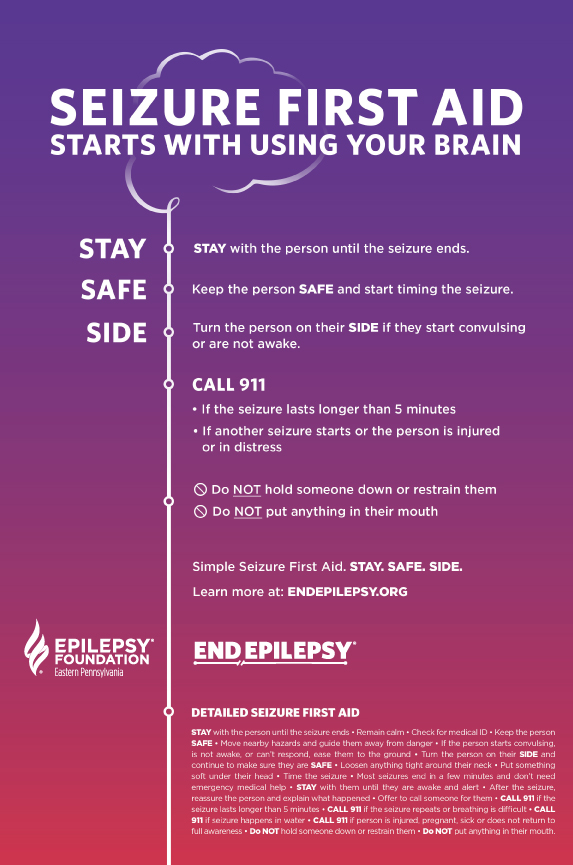
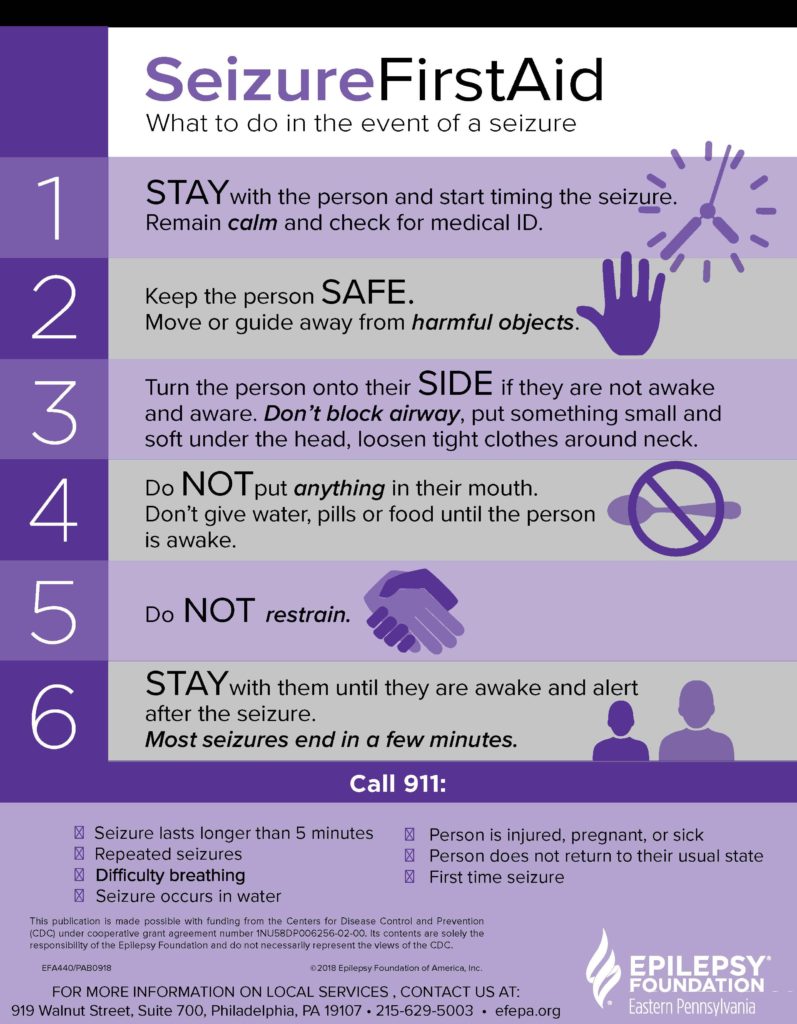
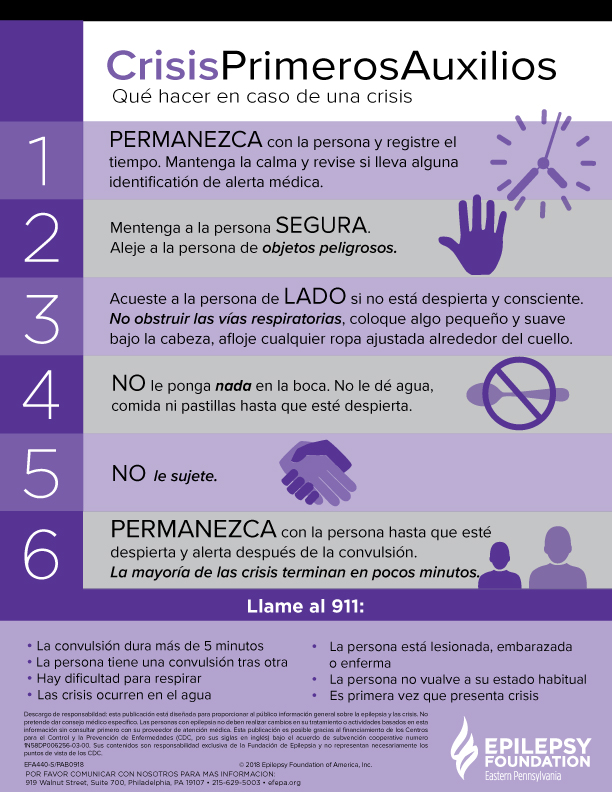
Seizure first aid varies for each type of seizure. It is not difficult but can easily be mishandled. To keep a person who is having a seizure safe and comfortable, take a moment to learn proper first aid for seizures.
Home Safety
Many apartments or homes must be changed a bit to make them safe for people who have seizures. Many of these changes are simple and do not require much time or money. If significant changes are necessary, be sure to contact the landlord or property manager before making the changes. These simple fixes can result in a significant increase in safety:
- First, do a walk-through of the rooms to spot potential dangers. Note any sharp corners on furniture and counters, floors that can get slippery, or places that can get hot like fireplaces and stoves. Also, places with staircases and pools present unique concerns.
- General Precautions– Floors in all rooms should be covered in a dense pile carpet to protect from falling injuries. Also, pad any sharp corners that may be hit during a fall or seizure. Be sure that all walkways are clear of obstacles.
- The Kitchen– Use appliances that have an ability to shut off automatically when not in use. Try and use a microwave oven instead of a stove for cooking. If you are using a stove try and use electric over gas, as well as using the back burners to prevent burns if a seizure occurs. Plastic containers should be substituted for glass that may shatter.
- The Bathroom– Bathroom doors should open outward, not inward in case of a bathroom seizure. Install a shower seat, non-slip strips, and grab bars in the tub. Use shatterproof glass for mirrors and shower doors. Be mindful of water temperature settings to prevent scalding. Keep the bathtub drain flowing freely and always keep tub water levels low.
- Living Alone– Keep doors securely locked if wandering during a seizure is a concern. Avoid climbing on ladders or chairs. Use a “buddy system” and have someone call each day to ensure that contact is frequent. Pre-program important phone numbers. Subscribe to a personal care hotline such as Lifeline in case of emergency. Keep floors clear of clutter. Place barriers in front of any items that may get hot such as stoves and radiators. When using portable heaters or other appliances, make sure that they can’t tip over and have automatic shut-off switches. Using chairs that have arms can be a small but useful way to remain safe during a seizure.
For additional tips on safety and living along visit epilepsy.com or download this brochure!
To watch a 2022 webinar on Maximizing Safety and Independence at Home click HERE! For resources from this webinar click HERE!
Treatment of Epilepsy
When the doctor has made a diagnosis of seizures or epilepsy, the next step is to select the best form of treatment. If the seizure was caused by an underlying correctable brain condition, surgery may stop seizures. If epilepsy — that is, a continuing tendency to have seizures — is diagnosed, the doctor will usually prescribe regular use of seizure-preventing medications. If drugs are not successful, other methods may be tried, including surgery, a special diet, complementary therapy or vagus nerve stimulation (VNS). The goal of all epilepsy treatment is to prevent further seizures, avoid side effects, and make it possible for people to lead active lifestyles.
There is no cure for epilepsy, yet. Medications do not cure epilepsy in the same sense that penicillin can cure an infection. For many people with epilepsy, however, the medication will prevent seizures as long as they are taken regularly; but, successful drug therapy requires the active cooperation of the patient.
Antiepileptic drugs successfully prevent seizures in at least fifty percent of all patients for substantial periods of time. Another thirty percent enjoy a significant reduction in the number of seizures. Unfortunately, some people continue to have seizures regularly despite taking medication. For them, surgical or, in children, dietary therapy with the ketogenic diet may be helpful. There is also hope that continuing research will produce new drugs and new ways of using them that will eventually give seizure relief to everyone who has epilepsy.
Most epilepsy medicines are taken by mouth. The doctor’s choice of which drug to prescribe depends on what kind of seizure a person is having. People react to medicines in different ways. Some experience side effects, others may not. Some people’s seizures will respond well to a particular drug while someone else will have seizures that continue. It may take some time to find exactly the right dose of the right drug for each person with epilepsy.
Whenever possible, doctors try to prevent seizures with a single medication. This is called monotherapy. However, some people may require polytherapy, the use of more than one medication to achieve seizure control. When selecting a drug, your doctor will consider the type of seizures you have. Not all medications work for all types of seizures.
Like all drugs, epilepsy medicines have side effects. Some are dose-related, and become more likely as the dose increases.
Treatment Options
Medication
Ketogenic Diet
Vagus Nerve Stimulator
Surgery
Alternative Options
Sleep and Epilepsy
One of the most common questions we hear from people is about the relationship between epilepsy and sleep. Suffering from a sleepless night can impact seizure activity, and vice versa. For an overview of this issue and more, view the presentation below given by Dr. Camilo Gutierrez from the Temple Comprehensive Epilepsy Center.
Mood and Memory
Mood disorders are treatable medical conditions in which the emotional symptoms are intense, long lasting or recurrent and decrease the ability to function. Mood disorders may affect things like sleep, appetite or sexual desire and may start in response to a life stressor or may come for no apparent reason. People with mood disorders are not able to make themselves better through will-power or by “trying harder.”
Major depression and dysthymia are the most common mood disorders experienced by people with epilepsy. Some people with epilepsy experience milder forms of depression that affect their quality of life and also respond to treatment.
Anxiety disorders are another group of common medical illnesses with psychological and behavioral symptoms. Often people with a mood disorder also have difficulty with anxiety and for improvement both issues must be addressed. Depression affects about 18 million people in the U.S. and anxiety disorders affect about 19 million. The GOOD NEWS is that there are effective treatments for mood and anxiety disorders that help people feel and function better.
What Is Depression?
Depression is a medical illness that affects the body, mood and thoughts. It promotes an unrealistic negative view of one’s self and the world. Depression can make you feel like you have less energy. Things you normally found fun may not interest you anymore. There are several types of depressive disorders. Major Depressive Disorder (also called Major Depression) and Dysthymia are the most common in general and in people with epilepsy. From studies in the general community, approximately 1/3 of individuals with epilepsy suffer from depression symptoms. Among individuals with severe uncontrolled seizures evaluated at specialty epilepsy centers, rates of depression symptoms may exceed 50%.
What Is Anxiety?
Anxiety disorders are medical illnesses that cause people to experience irrational excessive fear and dread. Physical symptoms such as rapid heartbeat, stomach or chest pain, or shortness of breath. Anxiety disorders are different from the mild temporary anxiety that most people have when stressed. Anxiety disorders last at least 6 months and can get worse without treatment. Anxiety disorders often occur with other mental and physical illnesses including epilepsy. It is not uncommon for anxiety disorders to be accompanied by substance abuse and depression.
Do Mood Disorders Occur in Children With Epilepsy?
Mood and anxiety disorders can also occur in children and may affect schoolwork and social functioning. The causes are similar to those in adults. Yet, depression and anxiety are often overlooked in children with epilepsy because children with depression may not have all the same symptoms as adults. For example, depressed children tend not to lose their appetite or complain of tiredness and/or inability to sleep, but often develop new physical complaints, such as headaches or stomach pain. They may not express feelings of sadness, hopelessness or helplessness as easily as adults. Behavioral problems are very common symptoms of depression in children. Depressed children may be irritable, easily tearful, and angry. You may see more problems in school with attention and learning, he or she may spend less time with friends and family or stop activities they used to find fun.
Children with anxiety are chronic worriers. They worry about routine, everyday activities, and often seem very pessimistic. They frequently complain of headaches, stomachaches, and lethargy. They can be irritable and defiant when pushed into anxiety provoking activities. They also have difficulties separating from their parents and are fearful, particularly at night.
What Are the Signs That An Adult or Child Needs Treatment?
Everyone has occasional symptoms of depression or anxiety. These feelings become a mood disorder when they last so long or are so intense that they interfere with a person’s ability to function. It is important to share this information about yourself or your child with your doctor, who can help you assess whether they are severe enough to require treatment. Indications of a significant mood or anxiety disorder include problems at work or at school, spending less time with friends, doing fun things or interacting with others or increased use of alcohol and recreational drugs.
Relationship of Epilepsy And Depressive And Anxiety Disorders
People with epilepsy have a higher rate of depression and anxiety disorders than the general population. Often the same parts of the brain such as the amygdala and hippocampus that are involved in the generation of seizures are also involved in the development of anxiety and depressive disorders. Epilepsy can involve disruption in the chemical messengers (neurotransmitters) in the brain and this can be a factor in the development of depression and anxiety. Epilepsy can present many stressors such as the loss of driving, difficulty at work and fear of having a seizure at an inopportune time or place. These significant ongoing sources of stress can contribute to the development of anxiety and mood problems. The treatment of epilepsy can have a positive, neutral or negative impact on mood and anxiety.
Mood Problems Before, During, and After A Seizure
Before
Some people feel depressed, anxious or irritable hours or days before a seizure. The bad feelings get worse as the seizure gets closer and then are usually gone after the seizure. At this time, there is no recommended treatment except to work for better seizure control.
During
A simple partial seizure is caused by abnormal electrical discharges in one part of the brain and occurs when the person is conscious. Some simple partial seizures consist of an emotion because the discharges are occurring in a part of the brain that produces a feeling. One person may feel fear and another might feel a wave of depression or a thought of suicide. These might be recognized as seizures because the emotion comes suddenly out of the blue and the event is very similar every time it comes. Sometimes the simple partial seizure progresses to a complex partial seizure which confirms the diagnosis of epilepsy. Education about the correct diagnosis can be reassuring to a person with simple partial seizures. The treatment would be to continue efforts to obtain better seizure control.
After
In addition to feeling wiped out and tired after a seizure some people experience depression and anxiety in the period after the seizure. These feelings usually go away in 24 hours but can last longer. The depressed feeling can be severe and in some people lead to thoughts of suicide. Suicidal thoughts after a seizure are more common in people who have a history of major depression or bipolar disorder. The first approach to this problem would be to work toward better seizure control. There has not been enough research to determine whether antidepressant medication would be helpful but it can be tried for severe cases.
Epilepsy Treatment And Mood Disorders
Anti-Epilepsy Drugs (AEDs)
People respond differently to medication. A medication that is well tolerated by one person may present troubling side effects to another. All AEDs can trigger psychological symptoms in some people.
Some AEDs act as mood stabilizers and can have a positive effect on mood. These include valproic acid, lamotrigine, carbamazepine, and oxcarbazepine. A negative change in mood can follow the discontinuation of an AED that is a mood stabilizer The person with epilepsy may not have been aware that the medication was treating mood issues as well as seizures. The appearance of mood symptoms when a person with epilepsy is switched to a new AED should not necessarily be attributed to the effect of the new AED.
Some AEDs can have negative effects and contribute to feelings of depression, anxiety, irritability and frustration. Phenobarbital and primidone are associated with depression. An AED is more likely to cause depression in a person who has a prior history or family history of depression, anxiety or alcoholism.
A person who is on an AED that is known to have negative effects on mood may find that he or she feels much better after a change in medication.
You need to work closely with your doctor to be sure that you are on the best AEDs for you. You count on your doctor’s expertise but your doctor also needs you to provide the information needed to keep you on the best medications. An important issue is the timing of mood symptoms and changes in AEDs. You will be of great assistance if you present your doctor with a seizure calendar on which you record when you start and stop or change the dosage of AEDs, when you miss a dose, seizure occurrence, and a log of your moods.
Recognizing Mood Disorders
How Might Mood Problems Affect Me?
It may be a sign of a mood disorder if your moods are long lasting, intense or keep you from living a happy life. You may have a mood disorder if you have ongoing feelings of anxiety, depression or irritability, or have feelings of fear, panic, or pain that are not easily explained by your seizures or other medical causes. You may be aware of problems getting along with coworkers, family or friends. Your mood may change for a few days before or after a seizure. You may be irritable or depressed without realizing it. You may get angry without reason. You may have physical symptoms such as headaches, chest or stomach pain. Ask people who know you well to help you by providing their view of your behavior and mood.
If you have mood symptoms that affect your usual activities, tell your doctor and consider seeing a mental health professional to be screened for mood disorders. Sometimes, AEDs and brain dysfunction can cause similar symptoms and mimic mood disorders. A health professional can help you sort out the cause of your feelings. The impact of mood disorders on your life is at least as important as your seizures and should receive the same attention to treatment. Do not hesitate to bring up this subject during an office visit.
Can Mood Problems Lead to Alcohol or Drugs?
Sometimes people use drugs or alcohol to feel better. They may not even realize they are doing this. Alcohol or drugs provide only temporary if any relief from mood problems. Alcohol and drugs may increase seizure frequency, cause mood problems or make mood problems worse. Ask your doctor to help you assess the situation. Some people benefit from treatment for substance abuse as well as treatment for mood disorders
Can Mood Disorders Result in Suicide?
Sometimes people with depression think about suicide. Feelings of hopelessness brought on by the depression may make it seem that things will never get better. Suicide is more common in people with epilepsy than the general population because of their increased stressors. If you are thinking about harming yourself or killing yourself or know someone who is:
ALWAYS REACH OUT FOR HELP! TELL SOMEONE WHO CAN GET HELP RIGHT AWAY
1. Seek immediate medical or mental health attention.
2. Go to an emergency room of a hospital
3. Call 911
4. Call 1-800-273-TALK (8255) 24 hour toll free, National Suicide Hotline
If you are concerned about another person, always take their statements about suicide seriously.
Children and adolescents with epilepsy also experience thoughts of wanting to die or hurt themselves, particularly if they are having emotional, behavior, learning or social problems. Currently, there is no evidence that AEDs cause suicidal thoughts and behavior in children and adolescents. But children often find it difficult to share suicidal thoughts with their parents. So, it is important to have children with mood, anxiety, learning and social problems evaluated by a mental health professional early on in the treatment of their epilepsy. This information not only helps your child’s doctor treat the seizures, it also determines if your child also needs therapy and/or treatment with medications for depression and anxiety. Early treatment for these problems helps your child and you deal with all aspects of the illness.
How Can I Deal with Mood Problems When I Already Have Epilepsy?
If you have supportive family and friends, tell them how they can help you. It can also help to communicate with the many other people who are facing similar issues. A great place to start is by attending one of our 10 area support groups.
It may seem unfair to have to manage more than one problem. Because seizures often occur in the same parts of the brain that affect the emotions, for many people mood problems are very much a part of having epilepsy. It is important to recognize mood problems because effective treatment is available that can improve your quality of life. Doctors and other health care providers are becoming more aware of the importance of mood problems to people with epilepsy and are prepared to help. Various kinds of treatment are available, including counseling, psychotherapy, and medication.
How Can I Help A Person Deal With A Mood Disorder?
The person with the mood disorder is not the only one affected. Family members and other concerned friends may struggle with their own feelings. Common and normal reactions are frustration, confusion, fear, anger or resentment. It can feel hopeless when you don’t know how to help or when your assistance is rebuffed. It is important to remember that you did not cause the mood disorder and you cannot cure it but your support and understanding can be invaluable.
As a first step, learn about mood disorders: the types, symptoms, support resources and effective treatments. Be a good listener which will require you to be accepting and nonjudgmental. Give loving support rather than advice. Let your loved one know that you care and will help. Ask directly what he or she needs.
Often people with mood disorders feel discouraged and lack energy and initiative to seek help. They may have a feeling that they should handle the problem without assistance and may not believe that treatment can help. They may not be aware that their feelings and behavior could be symptoms of a mood disorder. When this is the case, you may need to take an active role in helping them get assessment and treatment. You can offer to locate resources, speak to their doctor, and accompany them to appointments. Your continued support may be helpful to assist them to follow through with treatment. You may find it helpful to seek a support group or counseling for yourself.
Are There Treatments for Mood Disorders?
Many types of treatment are available for mood disorders. Psychotherapy and medication are the mainstays of treatment, which may be used separately or together. The goal is to completely eliminate your symptoms. The most common type of medication treatment is called an antidepressant, of which there are several kinds. Antidepressant medication works to stabilize neurotransmitters in the brain. Your doctor is most likely to prescribe a selective serotonin reuptake inhibitor (SSRI). It is important to remember that medications for mood disorders may require dose adjustments and may take several weeks before becoming fully effective. Just like AEDs, sometimes more than one antidepressant may need to be tried before getting good results. For most individuals with epilepsy, depressive symptoms usually respond very well to low doses of medication.
Psychotherapy is also called talk therapy or counseling. Most psychotherapy used today for mood disorders is brief and focused on your current life. You and the counselor will be active partners in work to assist you in making changes that will improve how you handle things in your life. Interpersonal Therapy and Cognitive Behavior Therapy are two types of psychotherapy that are effective in treating mood disorders. Interpersonal therapy deals with relationships in your life. Cognitive Behavior Therapy helps you change negative styles of thinking that are affecting your mood. You will learn skills to handle situations that are difficult for you.
For an in-depth look at the impact of epilepsy on your mood and memory, watch this video from the 2015 Lehigh Valley Epilepsy Education Exchange by Dr. Susan Ingram. Scroll to the 15 minute mark to get started!
Self Esteem
The connection between epilepsy and low self-esteem
There is no evidence that epilepsy per se causes low self-esteem. However, recent research suggests that people with epilepsy sometimes have difficulty forming relationships with others, possibly due to neurological damage to the temporal lobe. One study of patients with poorly controlled epilepsy found that 68 percent of subjects had no personal friends. People who lack the social support that friendships offer are likely to feel isolated; subsequently, these feelings of isolation may have a negative impact on self-esteem.
Experts also cite other possible reasons why people with epilepsy are prone to low self-esteem: family over-protection, which prevents individuals from developing independence and self-esteem; the perceived stigma that accompanies epilepsy and resultant negative self-image; and general personal dissatisfaction.
Low self-esteem in males with epilepsy (MWE) is particularly common during adolescence, a period of heightened self-consciousness that may be exacerbated by having epilepsy. Surveys indicate that adolescents whose epilepsy is well-controlled are less likely to suffer from low self-esteem than those who have frequent seizures.
Effects of low self-esteem
Low self-esteem can result in general dissatisfaction. It can also adversely affect specific aspects of life. For instance, low self-esteem may contribute to sexual problems, such as decreased libido. Low self-esteem may also be partially responsible for under-employment among MWE. A recent report by the Epilepsy Foundation documented that people with epilepsy have an unemployment rate of 25 percent. Among people whose seizures are poorly controlled, that rate approaches 50 percent.
For an overview of living with epilepsy, view this presentation by Dr. Sarah Schmitt from the 2015 Women’s and Men’s Conference.
Ways to improve self-esteem:
Controlling epilepsy
Controlling epilepsy may help improve self-esteem. One study found that in children with epilepsy who successfully underwent surgery, it not only alleviated seizures at a younger age, but also improved the psychosocial status of these individuals later in life.
Support Groups
Group interventions have proved beneficial as self-esteem boosters. For instance, a recent study demonstrated how adolescents with epilepsy benefited from a 6-week, structured psycho- educational group intervention. The intervention involved cognitive-behavioral strategies in which participants were encouraged to share their own experiences. Results showed that the intervention helped participants better understand their disease and engage in peer support. Post-intervention outcome measurements indicated an overall positive trend for quality of life improvement, suggesting that support groups would benefit MWE suffering from low self-esteem.
Stress management
Stress management has been linked to improvements in self-esteem and seizure control. Recent research indicates that, by increasing self-esteem, MWE may be able to manage stressful situations more effectively. Moreover, studies indicate that stress management may lead to improved seizure control in some MWE. Therefore, MWE who suffer from low self-esteem and anxiety may benefit by learning and practicing relaxation techniques. Examples of these techniques include aromatherapy, tai chi, reflexology and meditation.
Seeking professional help
If feelings of low self-esteem persist for a prolonged period of time or interfere with daily living, it is advisable to seek help from a trained professional, such as a clinical psychologist or a qualified counselor. A referral can be obtained through a primary care provider.
Headaches and Epilepsy
Caregivers: Helping Someone with Epilepsy
If someone in your life is diagnosed with epilepsy, it’s important to be supportive and understanding. You have already taken a great first step by visiting our website to learn more. Education is key to making our community safe for those with seizures.
But if you are a caregiver for someone with epilepsy, whether it is a child or an adult, it can be tough sometimes. Managing an epilepsy diagnosis is often emotionally difficult. If you’re feeling stressed or overwhelmed, we encourage you to attend one of our support groups or social events. Finding others that have shared the same experiences as you can be so helpful.
We also hope you’ll view the slides below, presented at the 2014 Epilepsy Education Exchange. It provides a great overview of how to help take care of YOU, while you take care of your loved one with epilepsy.